In December 2022 – month 24 of the project – SIMCor has delivered the proof-of-principle of its virtual cohort generator, namely its methodology for generating populations of ‘virtual’ (mathematical model-based) patients, as well as preliminary results on the use of such models for the clinical evaluation of cardiologic implants through computer-based simulations. The work has been led by researchers from the Eindhoven University of Technology (TUE), Netherlands, with the collaboration of the entire consortium.
The virtual cohort generator, by definition, is a pipeline of mathematical models able to generate virtual reproductions of human patients’ anatomy and physiology, and filter them using a multi-step strategy to obtain a population of high-fidelity ‘virtual patients’, able to accurately reproduce not only real patients’ features, but also their response to a device-based treatment of interest, mimicking the process of a real clinical trial.
The virtual cohort generator has been integrated in the project virtual research environment (VRE), a data repository and computing space developed for the generation of virtual cohorts and the conduction of simulated (‘in-silico’) biomedical device trials.
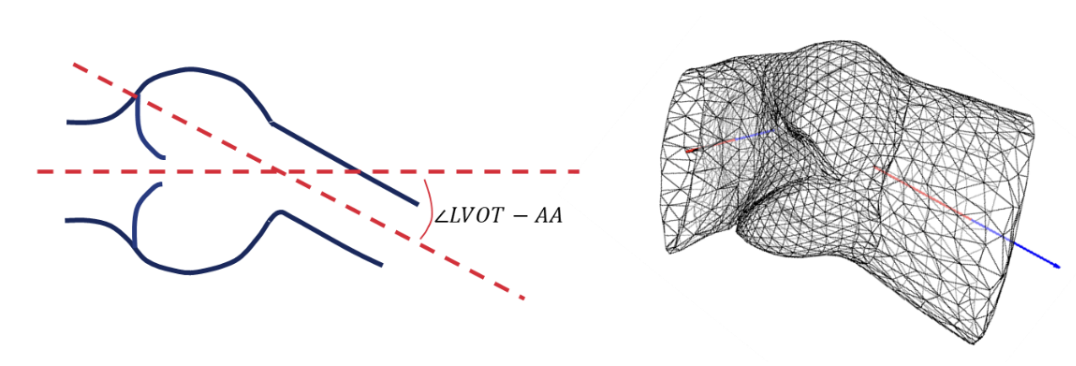
The methodology for generating and validating virtual cohorts is a multi-level process highly dependent on the type of disease and the medical device under evaluation. First, stakeholders shall define the patients’ physiological and anatomical features, as well as the properties of the medical device, to be evaluated in the simulated trial (the ‘output of interest’ or ‘output space’). Then, modellers analyse the not entirely known numerical distributions and variability of real patients’ data of interest (the ‘input space’), and develop mechanistic models able to reproduce these distributions in the virtual cohort (‘model templates’). The numerical distributions produced by the virtual cohort generator are then filtered, in order to include only those virtual patients that are realistic compared to a real patient population’s distribution, based on clinical knowledge.
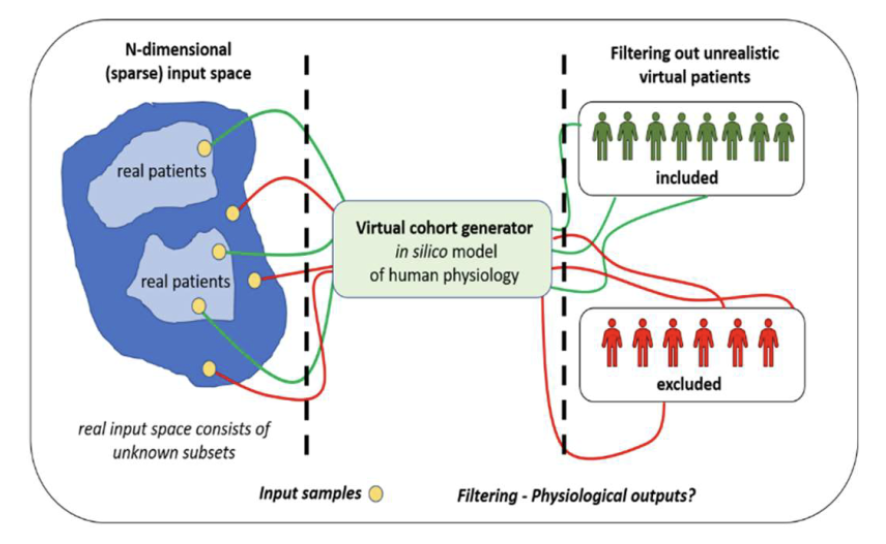
The validation of the generated virtual cohorts follows, articulated in three steps. The (1) patient-specific validation is used to demonstrate that the mechanistic model can realistically mimic the physiology of real patients. The (2) self-validation uses a sub-population of the real patient cohort – previously set aside – to assess whether the numerical distributions of the virtual patients mimic the real distributions used to create the virtual cohorts. Finally, in the (3) cross-validation, the outputs of interest of the virtual cohorts in the in-silico clinical trial are compared with independent patient cohorts of analogous real clinical trials, to verify whether the numerical outputs from the in-silico trial are comparable with real clinical trial outputs.
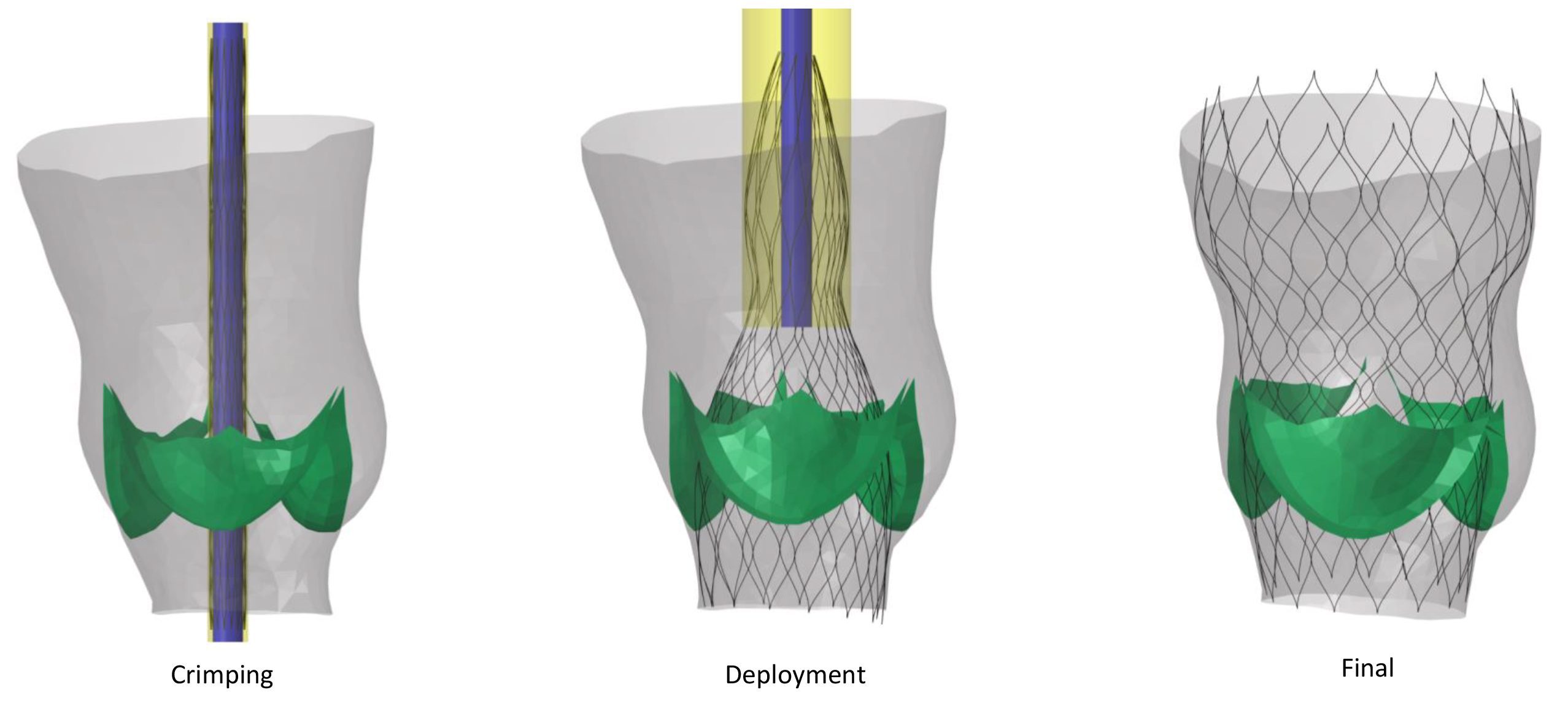
SIMCor focuses on cardiologic diseases and device-based treatments. Particularly, on aortic valve stenosis and its treatment using transcatheter aortic valve replacement (TAVR), and heart failure, monitored using a pulmonary artery pressure sensor (PAPS).
The initial proof-of-concept validation of the virtual cohort generator has been successfully conducted on the generation of synthetic geometries of the ascending aorta and left ventricular outflow tract of aortic stenosis patients using filters defined by clinical requirements, as well as on the exemplary transcatheter aortic valve implantation (TAVI) and the assessment of device effects on the virtual patient population. Further assessments will be conducted in the next months to validate the reliability of the method to mimic larger cohorts of real patients from independent clinical trials.